You’ve made the courageous decision to taper off Suboxone and reclaim control of your life. Maybe you’re tired of daily doses, concerned about long-term use, or ready for full independence from medication-assisted treatment. But attempting how to get off Suboxone at home without a plan often backfires—triggering weeks of brutal withdrawal that sabotage recovery. The truth? Successful home tapers require medical supervision, precision dosing, and strategic symptom management, not willpower alone. This guide reveals the exact physician-approved protocol for tapering Suboxone safely at home while minimizing suffering and protecting your hard-won sobriety.
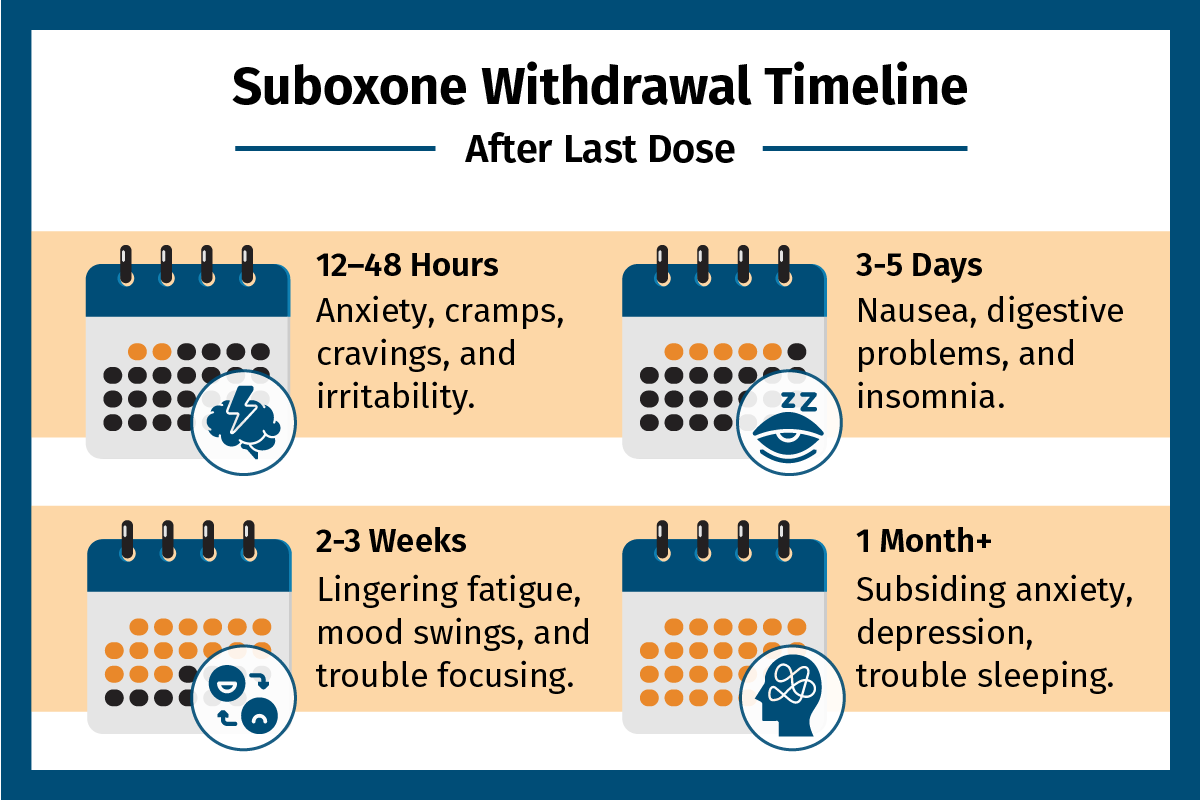
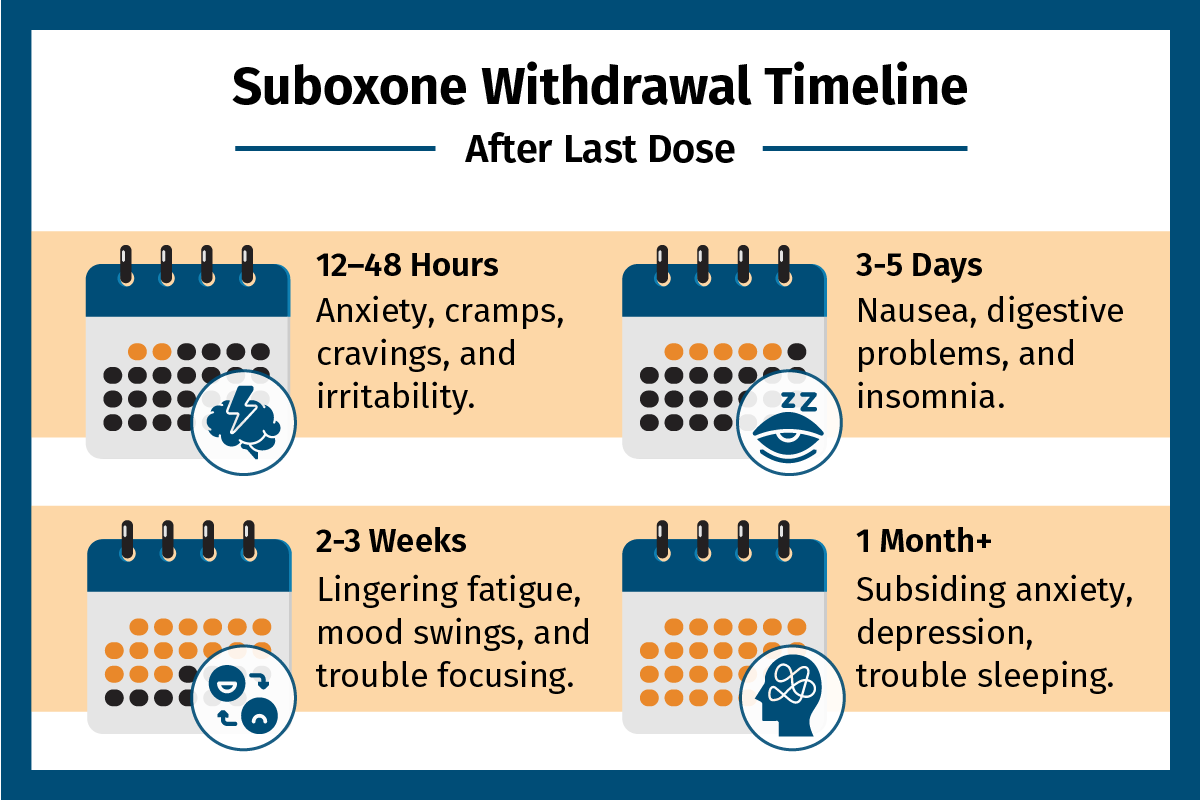
Most people underestimate Suboxone withdrawal because buprenorphine’s 36-hour half-life creates a slow-building storm. Unlike short-acting opioids, symptoms peak days 3-7 but can linger for months through post-acute withdrawal syndrome (PAWS). Rushing the process increases relapse risk by over 800%. But with the right approach—a 3-12 month physician-guided taper, daily tracking, and targeted comfort medications—you can navigate this journey with dignity. Let’s build your personalized exit strategy.
Why Suboxone Withdrawal Lasts Longer Than You Expect
Buprenorphine’s unique pharmacology explains why quitting cold turkey fails. As a partial opioid agonist, it occupies brain receptors for days, tricking your body into halting natural endorphin production. When you stop abruptly, your nervous system screams for relief—but recovery takes time. Withdrawal isn’t a sprint; it’s a marathon with distinct phases demanding different strategies.
The Hidden Timeline You Must Respect
- Days 1-2: Anxiety, yawning, and restlessness signal early withdrawal
- Days 3-7: Peak misery—vomiting, muscle cramps, and insomnia hit hardest
- Weeks 2-8: PAWS brings crushing fatigue, depression, and cravings
- Months 2-6: Gradual brain chemistry rebalancing occurs
Attempting to compress this timeline into weeks guarantees failure. Your taper speed must match your body’s adaptation rate—typically 5-25% dose reductions every 1-2 weeks. Ignoring this biological reality turns manageable discomfort into a relapse trap.
Doctor Partnership Essentials Before Tapering
Skipping medical oversight when learning how to get off Suboxone at home is like skydiving without a parachute. Your physician isn’t just prescribing medications—they’re your withdrawal navigator. Schedule telehealth check-ins every 2-4 weeks starting before your first dose reduction. During these critical visits, they’ll:
- Stabilize co-occurring conditions like anxiety or chronic pain first
- Prescribe comfort medications (clonidine for anxiety, gabapentin for muscle aches)
- Adjust taper speed based on your symptom tracker
- Provide emergency protocols for severe withdrawal
Home Preparation Checklist
- Remove all unused opioids from your house immediately
- Stock 2-week supplies of prescribed comfort meds and electrolytes
- Set up daily check-ins with a sponsor or trusted family member
- Download a withdrawal tracking app like “Narcan Ready” or use paper logs
- Post emergency numbers: 988 Suicide Lifeline, your doctor’s after-hours line
Pro Tip: Request a naloxone kit during your pre-taper visit—it’s free through many state programs and could save your life if relapse occurs.
Building Your Personalized Taper Schedule

Generic tapering charts fail because dependence depth varies wildly. A user on Suboxone for 6 months needs a different approach than someone on it for 3 years. Most successful home tapers follow this physician-supervised framework:
Moderate 19-Week Taper (Starting at 8mg Daily)
| Week | Dose | Critical Action |
|---|---|---|
| 1-2 | 8mg → 6mg | Monitor sleep quality; add magnesium glycinate |
| 3-4 | 6mg → 4mg | Start 15-min daily walks within 2 hours of dosing |
| 5-6 | 4mg → 3mg | Split dose AM/PM if nausea occurs |
| 7-8 | 3mg → 2mg | Introduce 4-7-8 breathing for anxiety spikes |
| 9-10 | 2mg → 1.5mg | Begin mindfulness practice upon waking |
Long-term users (>2 years): Double each phase duration. For doses below 1mg, switch to micro-tapers: dissolve 2mg films in 8ml water for precise 0.25mg doses. Hold each new dose 7-14 days—never reduce until withdrawal symptoms fully resolve.
Daily Symptom Tracking That Prevents Relapse
Your body sends warning signals you can’t afford to ignore. Rate these symptoms 0-4 twice daily:
– Physical: Sweating, muscle aches, nausea, diarrhea
– Mental: Cravings, irritability, depression, insomnia
Total Score Response Guide:
– 0-8: Continue taper schedule
– 9-16: Pause reductions; contact doctor
– 17+: Temporarily increase dose; seek immediate help
Red Flag Alert: Persistent vomiting beyond 24 hours or suicidal thoughts require ER care—don’t tough these out. Tracking isn’t optional; it’s your relapse radar.
Comfort Medication Protocol for Critical Symptoms
Prescribed adjuncts transform unbearable misery into manageable discomfort. Use these physician-approved combinations:
Withdrawal Symptom Triad Solutions
- Anxiety/Restlessness: Clonidine 0.1mg up to 3x daily (check BP first)
- Nausea/Diarrhea: Ondansetron 4mg every 8 hours + loperamide 2mg after loose stools
- Insomnia: Trazodone 50mg at bedtime—never benzodiazepines
Critical Warning: Taper comfort meds over 5-7 days after your final Suboxone dose. Stopping clonidine or gabapentin abruptly causes rebound symptoms that mimic withdrawal.
Lifestyle Supports That Actually Work
Medication alone won’t cut it. These evidence-based habits reduce PAWS severity by 40%:
- Hydration: 2-3 liters daily with electrolyte tablets during diarrhea
- Nutrition: Eat protein-rich meals every 4-5 hours (eggs, salmon, Greek yogurt)
- Exercise: 30-minute walks daily—boosts natural endorphins without strain
- Sleep Hygiene: Zero screens after 9 PM; cool, pitch-black room
Pro Tip: Set phone alarms for “urge surfing” when cravings hit: Breathe 4 seconds in, hold 7, exhale 8—repeat for 2 minutes while calling your sponsor.
Handling Relapse Without Self-Destruction
65% of taper attempts involve at least one relapse. Your response determines long-term success. If you slip:
- Don’t panic—this is part of recovery for most people
- Use your naloxone kit if opioids were involved
- Contact your doctor within 24 hours for dose re-stabilization
- Resume tapering at 25% slower speed after 3 stable days
Never try to “power through” after relapse—that’s when fatal overdoses happen as tolerance drops. Relapse isn’t failure; it’s data for your next attempt.
Post-Taper Recovery Plan That Sticks
The real work begins after your final dose. Protect your investment with:
- Naltrexone bridge: Start oral naltrexone 50mg daily 7-10 days after quitting
- Therapy schedule: Weekly CBT sessions for first 3 months
- Accountability: Monthly urine screens even if not required
- Peer support: 3+ recovery meetings weekly (NA, SMART Recovery)
Critical Insight: PAWS peaks at 2 months—don’t mistake normal brain healing for “failure.” Cravings will fade if you stick to the plan.
Final Reality Check: How to get off Suboxone at home successfully isn’t about speed—it’s about sustainability. Most who rush quit within weeks, while those honoring their biology succeed. Partner with your doctor, track symptoms religiously, and adjust based on your body’s feedback. Freedom from Suboxone requires patience, but with this protocol, you’ll trade temporary discomfort for permanent liberation. Your journey to true recovery starts today—not when you hit zero, but when you commit to doing this right.