Your father, a decorated Vietnam veteran, can no longer safely bathe or dress himself after his stroke. You’ve been managing his care alone, but you’re exhausted—and he’s too proud to ask for help. The good news? The VA offers comprehensive home health care programs that could provide the support both of you need, often at little to no cost. This guide walks you through exactly how to access these benefits, from determining eligibility to selecting providers—so you can get the home health care for veterans you’ve earned through service.
VA Home Health Care Eligibility: Do You Qualify?
Service Requirements for Immediate Eligibility
You qualify if you served in active military, naval, or air service—including activated Reserves or National Guard (non-training)—and received discharge under conditions other than dishonorable. This includes veterans who served stateside during peacetime, not just combat veterans. Critical requirement: You must be enrolled in VA health care benefits to access home health services.
Clinical Need Assessment Pathways
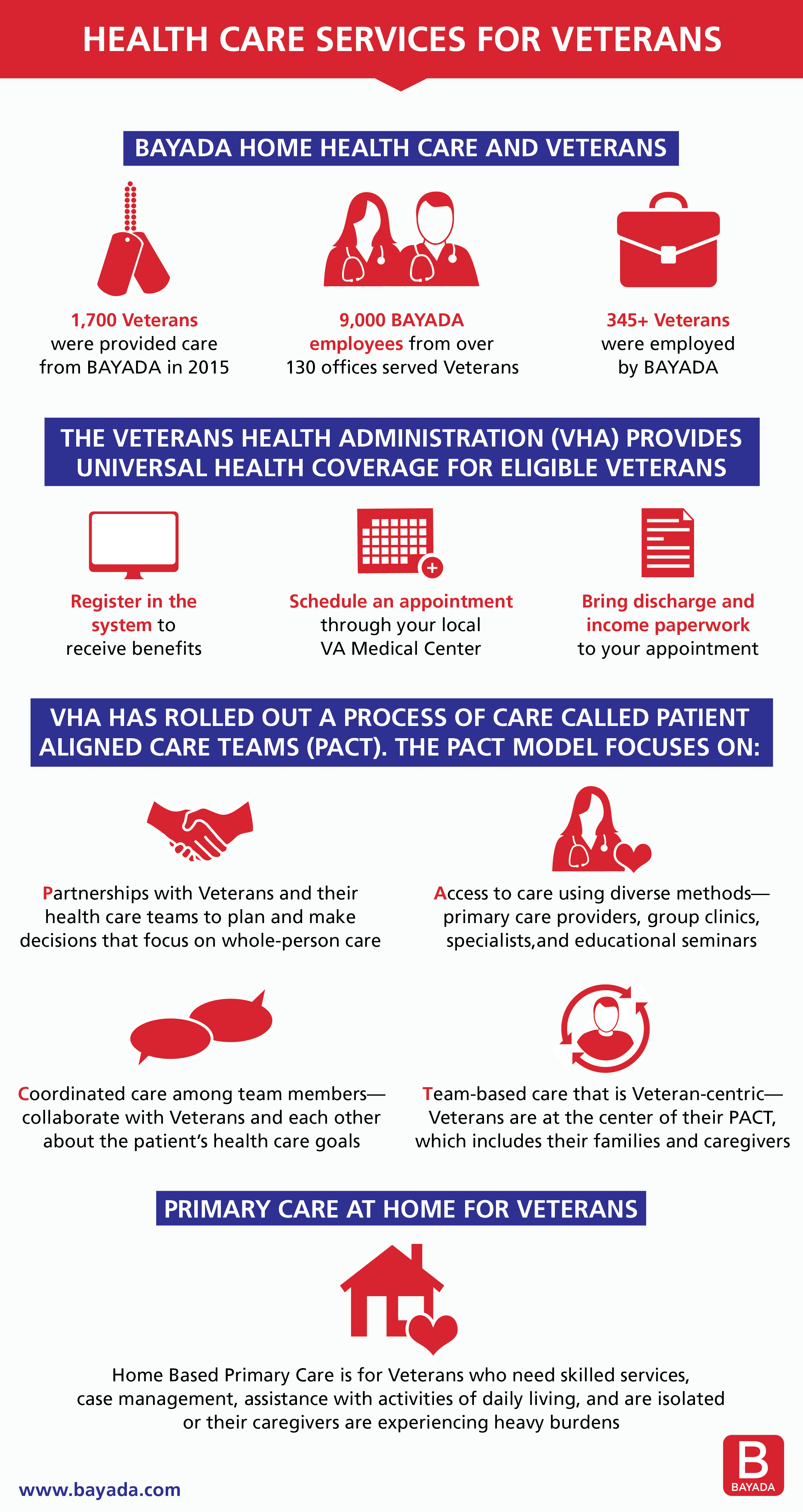
Your VA primary care provider will conduct a comprehensive geriatric evaluation to determine if you meet one of three clinical pathways:
- Primary Pathway: Need help with 3+ activities of daily living (bathing, dressing, toileting, eating, transferring)
- Cognitive Pathway: Significant memory or thinking problems affecting safety
- Combined Pathway: Need help with 2+ daily activities plus two additional factors like being over 75, living alone, or frequent hospital visits
Priority Group Impact on Coverage
Your priority group determines both eligibility and costs. Service-connected disabilities place you in the highest priority group, while higher-income veterans without service-connected conditions fall into lower priority groups. Warning: Higher priority groups receive faster approval and lower copays—verify your status before applying.
Top VA Home Care Programs for Veterans
Homemaker and Home Health Aide Care: Essential Daily Support
This foundational program provides community-based services under registered nurse supervision. Aides visit based on your needs—daily, weekly, or occasionally—and services continue as long as required.
Homemaker services include:
– Light housekeeping in patient-used areas (dusting, vacuuming, laundry)
– Meal preparation and grocery shopping
– Transportation to appointments
– Personal grooming assistance
– Social interaction and companionship
Home health aide services provide:
– Bathing, dressing, and toileting assistance
– Vital signs monitoring
– Medication reminders
– Mobility and transfer help
– Basic wound care under supervision
Home-Based Primary Care for Complex Medical Needs
HBPC serves veterans with serious medical conditions who cannot easily travel. A VA medical team brings primary care directly to your home, including care coordination, medication management, and chronic disease oversight. You must be enrolled in VA health care and meet clinical requirements to qualify for this intensive support.
Understanding Costs and Financial Benefits
Standard VA Coverage Breakdown
Most veterans pay little to nothing for home health care. Copayments vary based on your disability status and income, but care related to service-connected disabilities carries no copayment. For the Homemaker/Home Health Aide program specifically, the first 21 days each year have no copayment—after day 22, you’ll pay up to $15 daily (2023 rate).
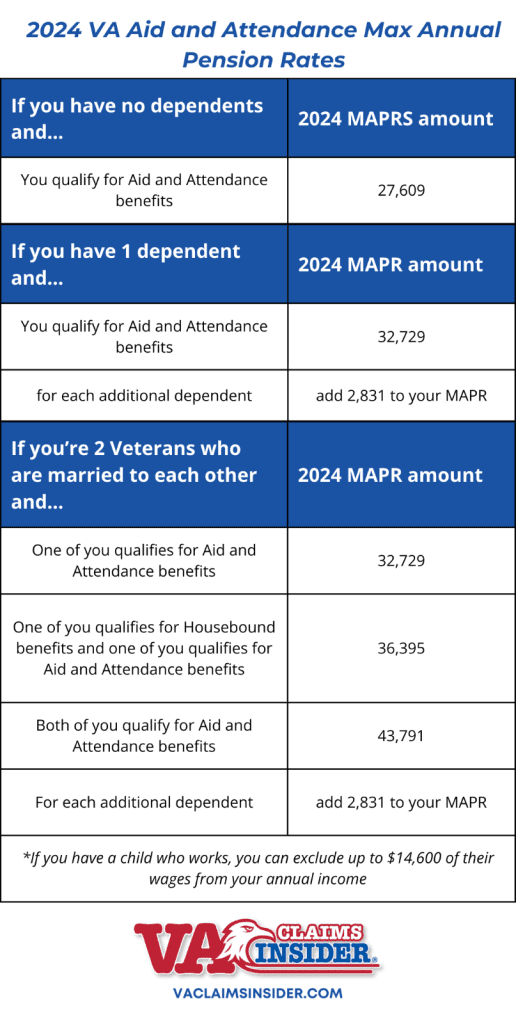
Aid & Attendance Pension Benefits: Significant Monthly Payments
Wartime veterans needing help with daily activities may qualify for substantial monthly payments:
– Single veteran: $1,794/month ($21,528/year)
– Veteran with spouse: $2,127/month ($25,524/year)
– Surviving spouse: $1,153/month ($13,836/year)
These funds can offset any care costs not covered by VA programs.
VetAssist Program for Immediate Care Access
Can’t wait for VA processing? VetAssist provides 0% interest loans to start care immediately, reimbursed later with your VA Aid & Attendance benefits. This includes a medical alert system with Alexa technology and ongoing compliance monitoring—no out-of-pocket costs required.
Step-by-Step Application Process
For New VA Health Care Applicants
- Complete VA Form 10-10EZ (health benefits application)
- Submit through multiple channels:
– Online at va.gov (fastest processing)
– Phone: 877-222-8387
– Mail to your nearest VA medical center
– In-person at any VA facility - Gather required documents:
– DD-214 discharge papers
– Recent financial statements
– Medical documentation from physicians
– VA Form 10-10EC for copay estimation
For Current VA Enrollees
- Contact your VA primary care provider to request a comprehensive geriatric evaluation
- Complete the assessment—be honest about your needs and limitations
- Receive doctor’s order for services if you meet clinical criteria
- Get referred to a CCN home care agency in your area
Critical Contact Numbers
- VA toll-free hotline: 1-877-222-8387
- Caregiver Support Line: 855-260-3274
- VA 24/7 line: 800-698-2411
- Local Caregiver Support Coordinator: Available at every VA facility
Selecting Your Home Care Provider
VA Community Care Network Selection Process
The VA’s five regional networks connect you with state-licensed, CMS-certified providers. VA staff will help identify local agencies, considering your preferences when possible.
National approved networks include:
– Nurse Next Door (Texas and California markets)
– Right at Home (Atlanta area through Optum)
– Visiting Angels
– Veterans Home Care (VetAssist Program)
Essential Provider Evaluation Checklist
When selecting your care provider, verify:
– State licensing and insurance coverage (non-negotiable)
– Staff training programs and background checks
– References from other veteran families
– Service availability and emergency response times
– Payment plan compatibility with your VA benefits
Special Situations and Exceptions
Surviving Spouse Benefits Clarification
Surviving spouses of wartime veterans may qualify for Aid & Attendance benefits even after remarriage—unlike TRICARE, which terminates benefits upon remarriage. This critical distinction provides crucial financial support for home care needs when your spouse has passed.
Dementia Care Pathways for Veterans
Veterans unable to attend VA clinics due to severe illness can access home-based primary care. Specialized dementia day programs also provide daytime supervision while caregivers work or rest, offering essential respite for family members.
Essential Documentation Checklist
Required Paperwork for Fast Processing
Before starting your application, collect:
– DD-214 (discharge papers)
– Financial statements (income and net worth verification)
– Medical documentation (physician assessments)
– VA Form 10-10EC (Extended Care Services application)
Timing Strategy for Immediate Needs
Apply before you need care—processing can take weeks or months. For immediate needs, the VetAssist Program provides interim funding while your VA application processes. Pro tip: Submit applications online for fastest processing (typically 3-5 days faster than mail).
Caregiver Support Resources You Need
Family Caregiver Financial Assistance
The Program of Comprehensive Assistance for Family Caregivers (PCAFC) offers financial assistance to primary caregivers who are family members or live full-time with the veteran. Caregivers must be 18+ and complete required training to qualify for this lifesaving support.
Respite Care Options to Prevent Burnout
Prevent caregiver burnout with up to 30 days of respite care annually. Options include:
– In-home professional care
– VA-contracted community living centers
– Adult day health centers
Getting home health care for veterans involves navigating multiple programs, but the benefits far outweigh the effort. Start with your VA primary care provider for assessment, then use this guide to select the programs that best fit your needs. Remember—you served your country, and these benefits are your earned right, not charity. With the right documentation and support, you can secure the home health care for veterans that provides dignity, safety, and independence in your own home.