When your aging parent struggles to bathe safely or you need skilled nursing after surgery but can’t stay in the hospital, you’re not alone. Over 12 million Americans rely on home care services annually, turning their houses into safe, supportive environments where professional help comes directly to their door. Understanding exactly how home care works—what services you qualify for, who provides them, and how to pay—can transform overwhelming confusion into a clear path forward for you or your loved one’s care needs.
Home care offers a crucial bridge between hospital-level medical care and independent living, allowing people to recover or manage chronic conditions in the comfort of home. This guide cuts through industry jargon to show you precisely what happens when you request home care, from your first phone call to daily service delivery, so you can make confident decisions about your care options.
Personal Care vs. Medical Home Care: What You Actually Need
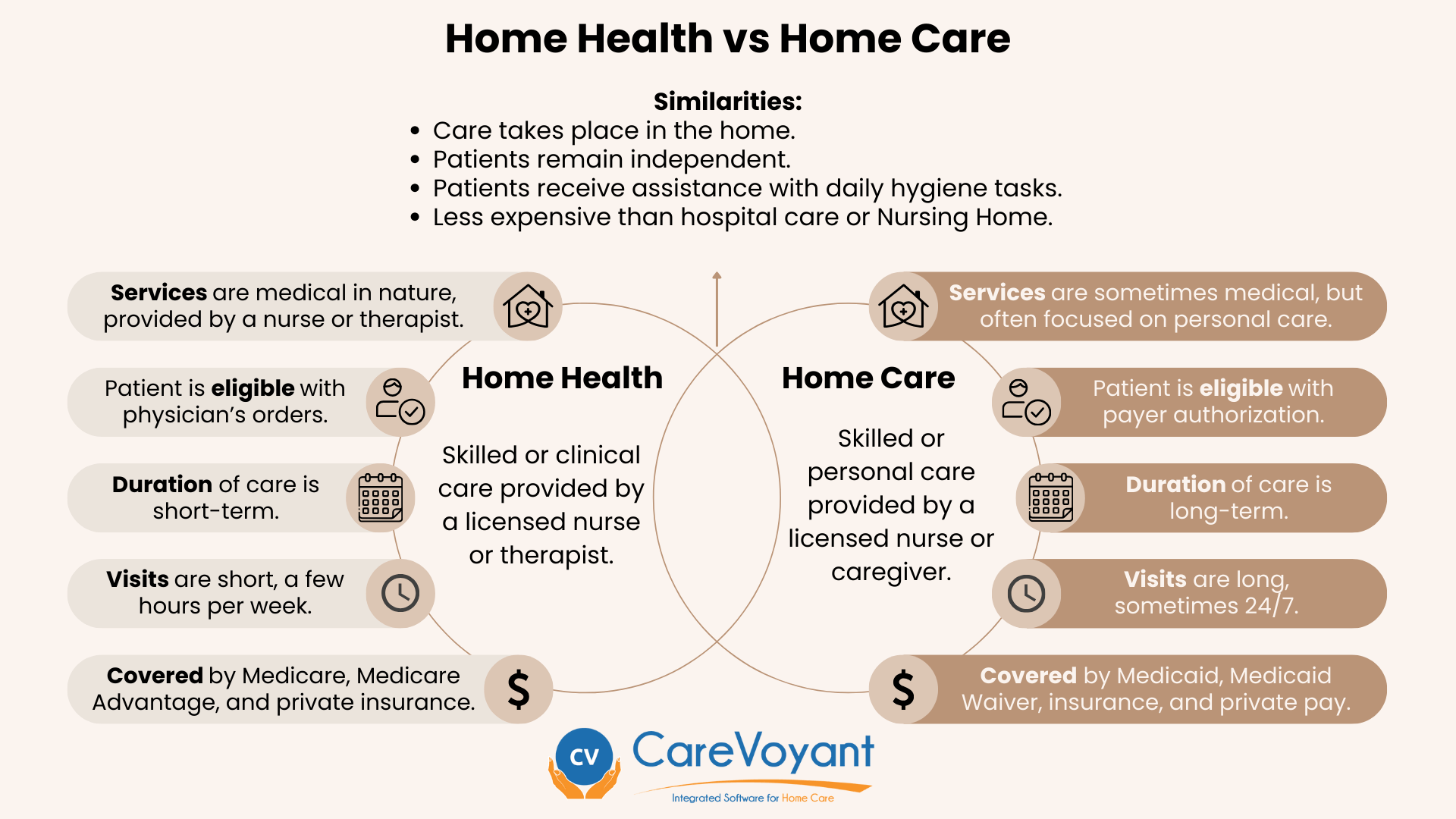
The first critical distinction in understanding how home care works lies in separating personal care services from medical home health care—confusing these leads to coverage denials and mismatched services.
Non-Medical Personal Care Services Explained
Personal care forms the backbone of most home care arrangements and requires no medical license to provide. These services focus on activities of daily living that become challenging due to aging, disability, or recovery. When you hire personal care, expect your caregiver to assist with bathing, dressing, meal preparation, light housekeeping, transportation to appointments, and medication reminders (without actually administering pills).
Key services include:
– Safe mobility assistance during transfers from bed to chair
– Grocery shopping and nutritionally balanced meal preparation
– Companionship to combat isolation through conversation and activities
– Light cleaning to maintain a safe, hazard-free living environment
Unlike medical care, personal care doesn’t require a doctor’s order, making it accessible for anyone needing daily support.
Medical Home Health Care Requirements
Medical home care operates under strict guidelines—this isn’t just someone checking blood pressure. When you qualify for home health care, licensed professionals like registered nurses, physical therapists, or speech therapists come to your home after a physician’s formal order. These services treat specific medical conditions through wound care, IV therapy, rehabilitation exercises, or swallowing therapy.
To receive Medicare-covered home health care, you must:
– Be considered “homebound” (leaving home requires considerable effort)
– Have a doctor-certified need for skilled nursing or therapy
– Use a Medicare-certified home health agency
– Require intermittent rather than 24/7 care
Crucially, Medicare won’t cover personal care services like help with bathing or dressing—only skilled medical needs.
Caregiver Qualifications: Who’s Actually Entering Your Home
Knowing exactly who provides care and what they’re qualified to do prevents dangerous misunderstandings about service capabilities.
Non-Medical Caregiver Limitations You Must Know
Most personal care comes from caregivers without medical licenses. While they provide invaluable support with daily routines, they cannot legally administer medications, perform medical procedures, or give medical advice. Their training focuses on safety techniques for transfers, recognizing when to call for help, and maintaining dignity during personal care tasks.
Critical boundaries to understand:
– They can remind you when medications are due but cannot give pills
– They assist with bathing but cannot treat skin breakdown
– They monitor for changes but cannot diagnose medical issues
When hiring directly, verify agency training protocols to ensure proper safety instruction.
When You Need a CNA or Licensed Nurse Instead
Certified Nursing Assistants (CNAs) bridge basic care and medical services through state-certified training. They monitor vital signs, report condition changes to nurses, and provide enhanced mobility support. However, CNAs still cannot administer medications, treat wounds, or perform catheter care.
For actual medical needs like wound dressing, IV therapy, or complex medication management, you’ll need licensed nurses. Registered Nurses (RNs) handle advanced medical care, while Licensed Practical Nurses (LPNs) provide basic nursing under RN supervision. Always confirm specific caregiver qualifications match your required services.
Home Care Costs Breakdown: What Really Determines Your Monthly Bill
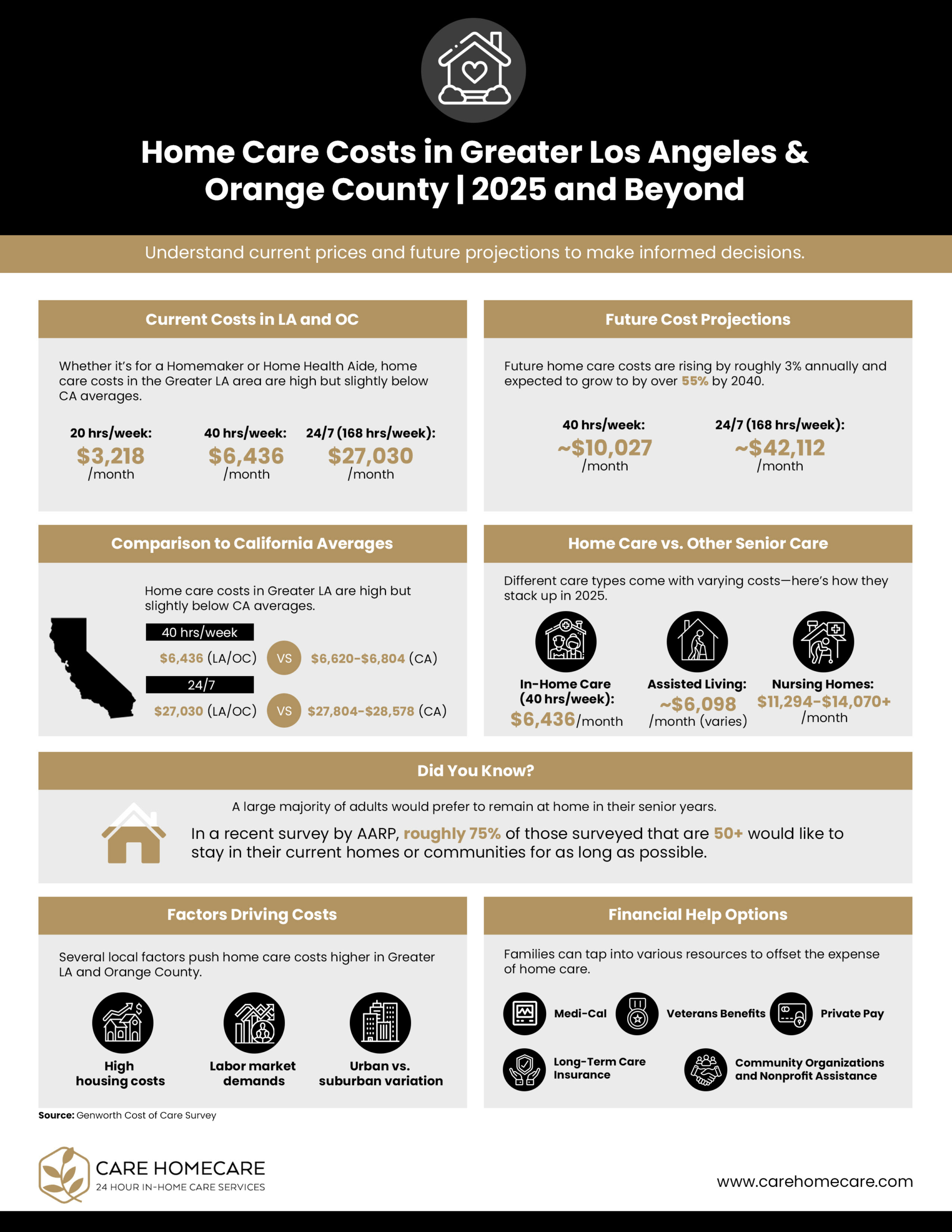
Your home care costs fluctuate dramatically based on service type, location, and caregiver qualifications—not understanding these factors leads to budget shocks.
Cost Drivers That Most Families Overlook
Personal care runs $22-$28 per hour on average, while skilled nursing can exceed $100 hourly. But hourly rates only tell part of the story. Geographic location significantly impacts pricing—urban areas often charge 25-40% more than rural regions. Care frequency matters too: 24/7 live-in care costs substantially less per hour than sporadic visits.
Unexpected cost factors include:
– Specialized dementia training adding 15-20% to caregiver rates
– Weekend or holiday surcharges of 25-50%
– Minimum visit durations (often 2-3 hours)
– Travel fees for remote locations
Always request a detailed cost breakdown before committing.
Payment Options That Actually Cover Home Care
Medicare covers only short-term skilled medical care after hospitalization—never long-term personal care. Medicaid coverage varies wildly by state, with some programs covering both medical and personal services for low-income seniors. Private insurance rarely covers non-medical care, though long-term care insurance policies may.
Alternative funding sources worth exploring:
– Veterans Aid & Attendance benefits for qualifying veterans
– State-specific Medicaid waiver programs
– Reverse mortgages or life insurance conversions
– Area Agency on Aging assistance programs
Most families combine multiple payment sources to manage costs effectively.
Service Delivery Process: What Happens When Care Begins

Knowing the workflow from your first inquiry to ongoing service prevents unpleasant surprises about how home care actually operates day-to-day.
The Critical First Assessment Most Agencies Rush
When you contact a home care agency, they should conduct a thorough in-home assessment—not just a phone questionnaire. This evaluation determines your specific needs, home safety concerns, and required caregiver qualifications. A proper assessment takes 60-90 minutes and involves you, family members, and sometimes your physician.
Red flags during assessment:
– Agency skips home visit for “preliminary” phone screening
– Assessor lacks medical background for health-related needs
– No discussion of emergency protocols
– Rushed timeline without family input
Insist on a comprehensive assessment before signing any agreement.
Daily Operations and Communication Protocols
Quality home care agencies implement clear communication systems so you’re never left wondering what happened during a visit. Expect daily written logs detailing services provided, condition observations, and any concerns. Modern agencies use digital platforms for real-time updates, photo sharing of completed tasks, and secure messaging.
Essential communication elements:
– Scheduled family check-in calls (weekly or bi-weekly)
– Emergency contact system with 24/7 availability
– Caregiver shift reports documenting handoff details
– Transparent incident reporting procedures
Ask specifically about their communication protocols before hiring.
Making Home Care Work Long-Term: Avoiding Common Pitfalls
Home care isn’t a one-time decision—it’s an evolving solution that requires proactive management to remain effective as needs change.
Warning Signs Your Home Care Isn’t Working
Most families don’t realize their care arrangement is failing until a crisis occurs. Watch for subtle indicators like caregivers consistently arriving late, incomplete service logs, or your loved one expressing discomfort with their caregiver. Unexplained bruises, weight loss, or medication errors signal immediate problems requiring intervention.
Critical warning signs:
– Caregiver making medical decisions without consulting professionals
– Missing personal belongings or unexplained financial activity
– Frequent caregiver changes without explanation
– Your loved one becoming withdrawn or fearful
Trust your instincts—if something feels wrong, investigate immediately.
Transition Planning for Changing Care Needs
Home care works best when you anticipate future needs rather than reacting to emergencies. Discuss progression protocols with your agency: how will services change if your condition declines? What’s their process for escalating care levels? When should you consider transitioning to assisted living?
Proactive planning steps:
– Schedule quarterly care plan reviews regardless of apparent stability
– Document changing needs through objective measurements
– Identify backup agencies in case your primary provider can’t meet evolving needs
– Involve your physician in regular care assessments
The most successful home care arrangements treat service levels as fluid rather than fixed.
Understanding how home care works empowers you to navigate this complex system confidently. Start by clearly identifying whether you need personal care assistance or medical home health services, then verify caregiver qualifications match your specific requirements. Scrutinize cost structures beyond hourly rates, explore all payment options, and prioritize agencies with transparent communication systems. Most importantly, view home care as an adaptable solution—regularly assess its effectiveness and adjust as needs evolve. With the right provider partnership and realistic expectations, home care becomes the practical, compassionate solution that lets you or your loved one maintain independence while receiving necessary support.